By: Cody Gramlich, Physiotherapist
You really don’t realize how fortunate you are to be able to perform simple day-to-day tasks until something limits you from these tasks. This thought has likely crossed your mind if you have ever had knee pain while running to catch  the bus, going up stairs at the office, or squatting to pick up your child. This hits close to home for me, as this was similar to what I was experiencing when I developed knee pain two months prior to running my first half marathon. With proper activity modification and management of the injury, I was able to complete the half marathon as planned! In this blog, you will learn about the presentation and management of one of the most common types of knee pain, patellofemoral pain syndrome.
the bus, going up stairs at the office, or squatting to pick up your child. This hits close to home for me, as this was similar to what I was experiencing when I developed knee pain two months prior to running my first half marathon. With proper activity modification and management of the injury, I was able to complete the half marathon as planned! In this blog, you will learn about the presentation and management of one of the most common types of knee pain, patellofemoral pain syndrome.
What is Patellofemoral Pain Syndrome?
Patellofemoral pain syndrome (aka runner’s knee) is an umbrella term for any long-standing knee pain behind your patella (kneecap) or around the patella. It has also been referred to in literature as runner’s knee or anterior knee pain. Runner’s knee is usually aggravated by any activities performed with your knee in a flexed position, usually while weight bearing. These activities include running, squatting, and stairs. However, your pain may also be aggravated by long periods of sitting. The common theme with all of these is that your knee is undergoing increased compressive forces in a flexed position2,5.
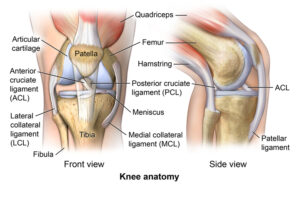
The patellofemoral joint is where your patella (kneecap) articulates with your femur (thigh bone). As you can see in the image above, there are a lot of structures that contribute to the stability and control of the knee and patellofemoral joint. This includes bony structures, ligaments, and muscles. However, stability and control of your knee is also significantly affected by positioning and control of your hip and ankle. So, when you see a physiotherapist, they will likely be addressing any dysfunction at all three of these regions.
Many mechanisms have been proposed as contributing factors to runner’s knee:
-
-
- Patellar maltracking
- Quadriceps weakness
- Hip abductor or external rotator weakness
- Foot pronation
- Muscular imbalance causing dynamic knee valgus
- Anatomical abnormalities
- Overuse or overloading
- Improper footwear
-
The literature tends to disagree or be inconclusive on the specific etiology of runner’s knee. Although, a common theme exists in that runner’s knee occurs as a result of biomechanical breakdowns at the hip, knee, and ankle. As a result, this causes a sensitivity in the patellofemoral region, but does not involve any conclusive structural damage.
Why is it Important to Understand Patellofemoral Pain Syndrome?
Patellofemoral Pain Syndrome is one of the most common knee pathologies,  especially for those of you who are runners. It is estimated to have an incidence of 3-15% in active populations and a prevalence of up to 23% in the general population3,4. In my personal caseload, I have treated this condition numerous times, both in adolescents and adults.
especially for those of you who are runners. It is estimated to have an incidence of 3-15% in active populations and a prevalence of up to 23% in the general population3,4. In my personal caseload, I have treated this condition numerous times, both in adolescents and adults.
When breaking down the stress your knee undergoes when running, it is easy to see why patellofemoral pain is more common in an active population. It is suggested that during running, the ground pushes back on your foot with forces of around 2.5x your bodyweight1. By the time this force is transmitted to the knee, the amount of compression by the quadriceps on the patellofemoral joint can be up to 4x your bodyweight1. This doesn’t mean you shouldn’t be running! This just means that it is important to identify and prevent functional breakdowns in your lower extremity that may lead to injuries associated with the high loads required by running. A physiotherapist or rehab professional will be able to help identify your areas of weakness and work to ensure you can be successful in your sports and leisure activities.
The good news is exercise therapy has strong evidence to support improving short and long term pain in individuals with runner’s knee2. Both strengthening exercises and running retraining have shown to have positive effects in terms of function3. One study suggested education on runner’s knee alone to be more effective than no management at all. The most effective intervention at a 3 month follow up was education combined with physical therapy6.
Taking a step further, recent literature suggests that a multimodal/individualized approach is necessary in treating runner’s knee, as  there are many contributing factors to the onset of the pain in the first place1,2. This should include education on taping and footwear. This should include managing beliefs/expectations on recovery. This should also include education on load/capacity, exercise, and run re-training1. A physiotherapist will be able to support you in most of these areas to give you an opportunity to get back to doing what you love.
there are many contributing factors to the onset of the pain in the first place1,2. This should include education on taping and footwear. This should include managing beliefs/expectations on recovery. This should also include education on load/capacity, exercise, and run re-training1. A physiotherapist will be able to support you in most of these areas to give you an opportunity to get back to doing what you love.
Some Risk Factors for Developing Patellofemoral Pain Syndrome2
-
-
- Frequent activity such as running, squatting, and stairs
- Overuse or sudden increase in physical activity level
- Quadriceps weakness
- Dynamic knee valgus (collapsing inwards)

- Patellar (kneecap) instability
- Foot abnormalities
- More common in female sex
-
*There is a variability and inconsistency in research when it comes to risk factors for developing runner’s knee. Some studies even suggest these issues may be a consequence of patellofemoral pain syndrome, not a cause. This further indicates a need for thorough assessment and multimodal treatment of your knee pain.
How Do I Know If I Have Patellofemoral Pain Syndrome?

-
-
- Knee pain is usually non-traumatic or gradual onset (although you may have a history of knee trauma/injury).
- Pain on the anterior (front) of the knee or around the patella (kneecap).
- You have high activity levels or a recent increase in activity levels.
- Knee pain with activity such as running, squatting, or stairs.
- Knee pain with prolonged periods of sitting while your knee is in a flexed/bent position.
- Knee pain typically does not have associated swelling or locking.
-
3 Strategies to Help Manage Your Patellofemoral Pain Syndrome Symptoms
1. Activity Modification
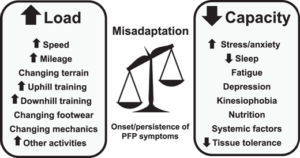
*Patellofemoral pain syndrome often occurs as a result of an imbalance between your body’s capacity and the loads it is undergoing with activity. A period of activity modification is likely necessary to manage this imbalance. If you are a runner, try a 1 minute jog, 1 minute walk cycle to see if your pain is better managed.
2. Quadriceps Rolling
*Tight quadriceps can contribute to patellar maltracking related to patellofemoral pain syndrome. Alternatively, quadriceps tightness can come as a result of your knee pain. Rolling will help decrease the tension on the front of your knee when it is in a flexed position. Try 2-5 minutes, 1-2 times per day.
3. Hip Strengthening (Glute Bridge)
*Strengthening the hip girdle will help with biomechanical alignment during dynamic activity such as squatting and running. This will help to decrease your knee pain with activity. Try 3 sets of 10-15 repetitions. You can do this with or without a band around your knees.
FAQ
How long does patellofemoral pain syndrome take to heal?
Healing timelines vary for patellofemoral pain syndrome depending on factors such as your age, activity level, and general health. Pain can often be alleviated with rest and stretching. However, changing the biomechanical breakdowns that contributed to your knee pain takes more time and effort. It is recommended to see a healthcare professional for recommendations to help resolve and prevent your symptoms.
Do I need surgery for my patellofemoral pain syndrome?
Typically, surgery is not required for patellofemoral pain syndrome, as there is no specific structural damage that is causing your pain. If other signs and symptoms exist such as direct trauma to the knee or persistent patellar dislocations, a referral for surgical consultation may be indicated.
What can I not do with patellofemoral pain syndrome?
There are no specific activities that need to be completely avoided with patellofemoral pain syndrome. However, many activities such as squatting, running, and stairs may further aggravate your symptoms. A short term period of rest followed by a gradual increase to full activity is recommended during recovery from patellofemoral pain syndrome.
What Comes Next?
Remember, patellofemoral pain syndrome is knee pain that occurs beneath or around your kneecap. It is one of the most common knee issues, especially for those of you who are active or run a lot. This type of knee pain is typically multifactorial and usually requires individualized management, depending on your specific presentation.
Start by trying some of the strategies listed above and see how it goes! Afterwards, it would benefit you to see a Peak Health physiotherapist to guide you through treatment, depending on your response.
Feel free to reach out if you have any additional questions on runner’s knee or you can book an appointment online by clicking here.
References:
-
-
- Esculier, JF., Maggs, K., Maggs, E., Dubois, B. (2020). “A Contemporary Approach to Patellofemoral Pain in Runners”. Journal of Athletic Training. 55 (12): 1206–1214. https://doi.org/10.4085/1062-6050-0535.19
- Gaitonde, D.Y., Ericksen, A., Robbins, R.C.; Dwight D. Eisenhower Army Medical Center, Fort Gordon, Georgia (2019). “Patellofemoral Pain Syndrome”. American Family Physician, 99 (2): 88-94, https://www.aafp.org/afp/2019/0115/p88.html?utm_medium=email&utm_source=transaction
- Neal, B. S., Barton, C. J., Gallie, R., O’Halloran, P., & Morrissey, D. (2016). “Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: A systematic review and meta-analysis”. Gait & Posture, 45, 69–82. doi:10.1016/j.gaitpost.2015.11.018
- Neal B.S., Lack S.D., Lankhorst N.E., et al (2019). “Risk factors for patellofemoral pain: a systematic review and meta-analysis” British Journal of Sports Medicine; 53: 270-281. https://bjsm.bmj.com/content/53/5/270
- Physiopedia 2021. “Patellofemoral Pain Syndrome”. Physiopedia. Accessed March 3, 2021, https://www.physio-pedia.com/Patellofemoral_Pain_Syndrome
- Winters M., Holden S., Lura C.B., et al. (2020). ”Comparative effectiveness of treatments for patellofemoral pain: a living systematic review with network meta-analysis” British Journal of Sports Medicine. doi:10.1136/ bjsports-2020-102819
-
Media References:
Knee Anatomy Picture:
-
-
- Comprehensive Orthopaedics, S.C. (2016). “Anatomy of the Knee”. Accessed March 3, 2021 via Google Image Search. https://comportho.com/anatomy/anatomy-of-the-knee/. [Original Source Unknown]
-
Load/Capacity Diagram:
-
-
- Esculier, JF., Maggs, K., Maggs, E., Dubois, B. (2020). “A Contemporary Approach to Patellofemoral Pain in Runners”. Journal of Athletic Training. 55 (12): 1206–1214. https://doi.org/10.4085/1062-6050-0535.19
-



 reach to grab a plate from the cupboard, or you can’t roll over at night to sleep on your side. This is what one client was struggling with before choosing to start physiotherapy. With a better understanding of his issue and how to manage it, he was able to return to playing pickleball up to five times per week without shoulder pain! One common cause of shoulder pain is commonly referred to as subacromial impingement, or subacromial pain syndrome. In this blog, you will learn what subacromial pain syndrome is, why it is important to understand, and what you can do to manage it.
reach to grab a plate from the cupboard, or you can’t roll over at night to sleep on your side. This is what one client was struggling with before choosing to start physiotherapy. With a better understanding of his issue and how to manage it, he was able to return to playing pickleball up to five times per week without shoulder pain! One common cause of shoulder pain is commonly referred to as subacromial impingement, or subacromial pain syndrome. In this blog, you will learn what subacromial pain syndrome is, why it is important to understand, and what you can do to manage it.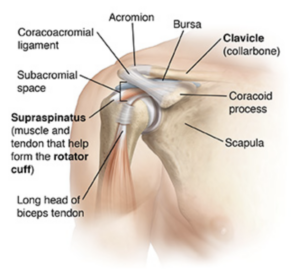
 Shoulder pain is common and can result in significant loss of function or participation in your day-to-day activities. It is suggested that up to 67% of community dwelling individuals may experience shoulder pain1. 44-65% of all reports of shoulder pain are thought to involve symptoms arising from the subacromial space1. Subacromial pain syndrome is a prevalent issue, so it is important to understand how to prevent and manage it.
Shoulder pain is common and can result in significant loss of function or participation in your day-to-day activities. It is suggested that up to 67% of community dwelling individuals may experience shoulder pain1. 44-65% of all reports of shoulder pain are thought to involve symptoms arising from the subacromial space1. Subacromial pain syndrome is a prevalent issue, so it is important to understand how to prevent and manage it. as the first-line treatment in subacromial pain syndrome6. A strong recommendation to include manual therapy as an integrated treatment was also made6. Another systematic review even suggested exercise to be as effective as arthroscopic surgery for subacromial pain syndrome3.
as the first-line treatment in subacromial pain syndrome6. A strong recommendation to include manual therapy as an integrated treatment was also made6. Another systematic review even suggested exercise to be as effective as arthroscopic surgery for subacromial pain syndrome3.

 If you have experienced or are experiencing nagging elbow pain, you know that it can significantly affect things such as sleep and your day-to-day activities (think… pouring a cup of coffee, lifting your child, working with hand tools, or playing your favourite sport). This was the story for a client of mine who developed elbow pain after a lot of lifting and carrying during a move. With some guidance and treatment for his issue, he was able to return to skiing weekly, without worrying about elbow pain every time he used his ski poles. If this sounds like something you have been struggling with, or you simply want to learn more, then keep reading! You will learn what tennis elbow is, what to look out for, and how to deal with it.
If you have experienced or are experiencing nagging elbow pain, you know that it can significantly affect things such as sleep and your day-to-day activities (think… pouring a cup of coffee, lifting your child, working with hand tools, or playing your favourite sport). This was the story for a client of mine who developed elbow pain after a lot of lifting and carrying during a move. With some guidance and treatment for his issue, he was able to return to skiing weekly, without worrying about elbow pain every time he used his ski poles. If this sounds like something you have been struggling with, or you simply want to learn more, then keep reading! You will learn what tennis elbow is, what to look out for, and how to deal with it.