Written by Kate Thompson, Physiotherapist
So You’ve Been Told You Have Osteoarthritis. You’ve Landed on The Right Page…
What Is Osteoarthritis?
Osteoarthritis (OA) is a disease that commonly affects joints of the body such as the hip and knee, shoulders and hands [1], and is a lot more common than people think. If we zoom into what is going on at the joint, it helps paint a picture of what is actually going on when an individual develops OA.
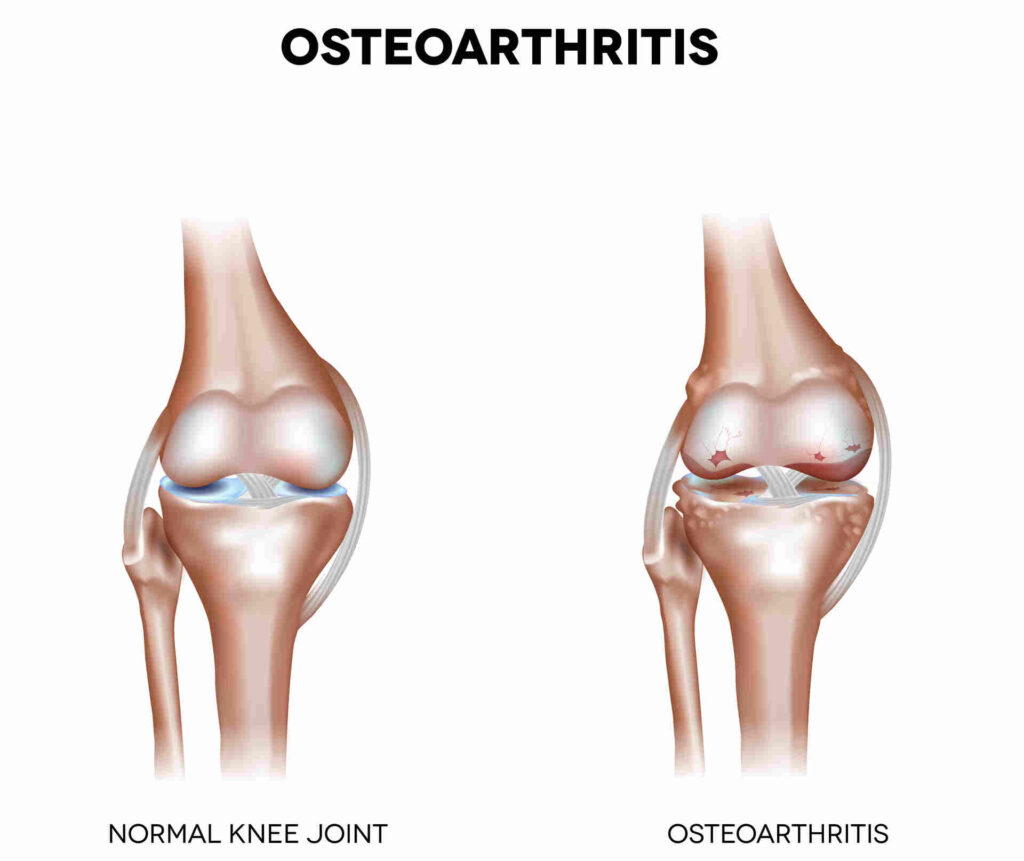
A joint is where two bones come together, and serve the function of absorbing and distributing mechanical load in your body [1]. A healthy joint should have cartilage covering the surface of the bones, enough space between the bones so they do not rub against each other, as well as ligaments and muscles surrounding them to support them and keep them stable.
OA results in changes to the cartilage, bone and joint space, and can also affect the surrounding ligaments, tendons and muscles [1]. As a result, the structure and function of the joint change which can result in symptoms such as pain, stiffness and instability [1].
“If you have knee osteoarthritis, you may feel unsteady when putting all of your weight through one leg while going down the stairs. This is because the muscles, ligaments, and joint structure are not able to support and disperse the weight of your body as it normally should.”
Who Is at Risk of Developing OA?
Known risk factors for developing OA include [1]:

- Aging
- Obesity
- Genetics
- Previous trauma/injury to the area
- Gender (females have a higher incidence than males)
- Hormones and metabolic disease
It is important to note, however, that OA is not inevitable if you have one of these risk factors! For example, although aging increases your risk of developing OA, not everyone who ages develops OA [1].
My Doctor Diagnosed Me With Osteoarthritis, but I Have Never Had an X-Ray. Do I Need One To Confirm the Diagnosis?
This is a tricky subject. In the past, it was common practice for health practitioners to refer patients for X-rays to guide the diagnosis of musculoskeletal conditions. Newer research, however, has identified that there may not always be a strong correlation between imaging findings and patient symptoms [2,3].
For example, if you took 100 people off the street and took an X-ray of their knees, some people without any knee pain at all may have X-rays that indicate OA, and some people with severe, debilitating knee pain may have X-ray results showing a healthy joint. In addition, if you are an older adult, it is common for there to be structural abnormalities found on your imaging that simply have developed over time and are not related to your symptoms at all [2].
Therefore, recent recommendations advise that OA should be diagnosed based on your symptoms, instead of through X-ray.
For example, if your symptoms follow a typical presentation of OA, such as joint pain, stiffness in the morning lasting <30 mins, crepitus with movement and weakness/instability, it is acceptable to be diagnosed without a referral for an X-ray [2,3].
Your doctor may request an X-ray if you have an atypical presentation and/or if there is suspicion of a different diagnosis2. Examples of an atypical presentation may include severe local inflammation, redness around the joint and rapid, progressive pain that is unrelated to use [2].
How Do I Know When I Need Surgery?
A better question might be, “How do I know if I need surgery?”. It’s important to consider that not everyone diagnosed with OA requires a joint replacement! It is recommended that patients diagnosed with OA try conservative management for a significant period of time to manage their symptoms, improve function and delay further changes to the joint structure [4].
The Osteoarthritis Research Society International suggests that NSAIDs (non-steroidal anti-inflammatory drugs) and exercise have the highest level of evidence for improving knee and hip OA symptoms [4]. If you have spent a significant amount of time trying conservative methods and still are unable to manage your pain, and your pain is considerably impacting your quality of life, it may be time to have a conversation with your doctor about other options.
Although there is significant evidence demonstrating that joint replacement surgery can improve symptoms, function and quality of life, surgical candidates are often under-educated about the risks of surgery and what the recovery process might look like [5]. For example, it can take months of physiotherapy to restore your mobility and strength following surgery.
Furthermore, you may still experience pain in the months following surgery as you progress through rehab to optimize your new joint function. In addition, there is a risk that you may not regain a full range of motion following surgery [5].
It is important to remember that everyone has a unique anatomy, fitness level, stress level, and life experiences going into surgery and all of these factors will play a role in your recovery. If you are currently waiting for surgery, it is important to consult with a Peak Health physiotherapist on how you can best prepare for the surgery to optimize your outcomes after the operation.
To learn more about Osteoarthritis, check out our other blogs on the topic or reach out to me directly at [email protected]! I would be more than happy to answer any questions you may have on how physiotherapy and exercise rehabilitation can help you manage your OA diagnosis.
To book a free discovery call with me, click here.
At Peak Health And Performance, we offer a wide range of treatment options including massage therapy to address a variety of conditions and help you get back to your daily activities pain-free. Some of the common conditions we can help with include:
- Poor posture
- Connective tissue issues
- Knee injuries
- Joint pain relief
References:
- He Y, Li Z, Alexander PG, Ocasio-Nieves BD, Yocum L, Lin H, Tuan RS. Pathogenesis of Osteoarthritis: Risk Factors, Regulatory Pathways in Chondrocytes, and Experimental Models. Biology. 2020; 9(8):194. https://doi.org/10.3390/biology9080194
- Xia Wang, Win Min Oo, James M Linklater, What is the role of imaging in the clinical diagnosis of osteoarthritis and disease management?, Rheumatology, Volume 57, Issue suppl_4, May 2018, Pages iv51–iv60, https://doi.org/10.1093/rheumatology/kex501
- Wood G, Neilson J, Cottrell E, Hoole S P. Osteoarthritis in people over 16: diagnosis and management—updated summary of NICE guidance BMJ 2023; 380 :p24 doi:10.1136/bmj.p24
- Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, Kraus VB, Lohmander LS, Abbott JH, Bhandari M, Blanco FJ, Espinosa R, Haugen IK, Lin J, Mandl LA, Moilanen E, Nakamura N, Snyder-Mackler L, Trojian T, Underwood M, McAlindon TE. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019 Nov;27(11):1578-1589. doi: 10.1016/j.joca.2019.06.011. Epub 2019 Jul 3. PMID: 31278997.
- Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012 Feb 22;2(1):e000435. doi: 10.1136/bmjopen-2011-000435. PMID: 22357571; PMCID: PMC3289991.
