Written By Dr. Sarah Gajecki
At Peak, we offer many different styles of needling techniques offered by a range of practitioners. The needling style and technique are dependent upon their specific training, and experience. I wanted to go over some common questions related to dry needling and acupuncture and shed some light on a few topics that often come up.
What Is The Difference Between Acupuncture and Dry Needling?
Dry needling is a practice that has been adapted based on Western medicine that involves the insertion of needles into trigger points of muscles and is based on the principles of anatomy and physiology. Acupuncture is based on meridians of energy and based on the principles of traditional Chinese medicine.
There are also many modernized forms of acupuncture that have integrated traditional concepts with a more modern and anatomical approach. The type of needling you will receive (whether it be acupuncture or dry needling) will depend on the training your provider has.
Does Dry Needling Use the Same Needles as Acupuncture?
Dry needling and acupuncture both use very small, thin stainless steel needles that are inserted at various depths depending on the targeted treatment area. The type of needle used in your treatment plan will depend on the area being treated and the style of needling being performed.
There are however overlaps in the types of needles used! The tool can be the same, however, the technique and delivery of the treatment can vary.
Can Dry Needling Cause Nerve Damage?
In rare instances, dry needling can injure a nerve or blood vessel. This can result in mild pain, numbness or tingling, all of which are temporary and normally dissipate quickly. The most common side effects of needling are just minor soreness or bruising.
What Are The Risks of Dry Needling?
Some minor risks of dry needling can include bruising, fainting, fatigue, very minor bleeding, and soreness. All of which are temporary and resolve quickly. In very rare instances a more serious and uncommon risk may occur, such as infection or a pneumothorax – but these occur very infrequently.
To mitigate those risks, we ensure only highly trained individuals perform these techniques and we only use single-use, sterile needles to prevent any risk of infection. Your practitioner will explain any potential risks to you at the time of your treatment, specific to the area you are having treated. Most commonly after a dry needling treatment, mild soreness is felt in those areas that were treated.
What Are The Benefits of Dry Needling?
Dry needling can be used to increase local blood flow to the target tissue and release muscle and soft tissue tension. Dry needling is also used to reduce pain by influencing the nervous system and stimulating the release of endorphins and serotonin.
Should I Avoid Certain Things After Dry Needling?
Following a dry needling session, patients should avoid icing the area that has been treated, stay away from alcohol and avoid overworking and stressing the area that has been needled. Heat can be beneficial after dry needling to aid with mild soreness and light exercise and movements is encouraged!
Where Is Dry Needling Most Effective?
Dry needling can effectively treat many musculoskeletal conditions. Commonly treated conditions that can be improved with dry needling include:
- Rotator cuff pain

- Iliotibial band syndrome
- Achilles tendonitis
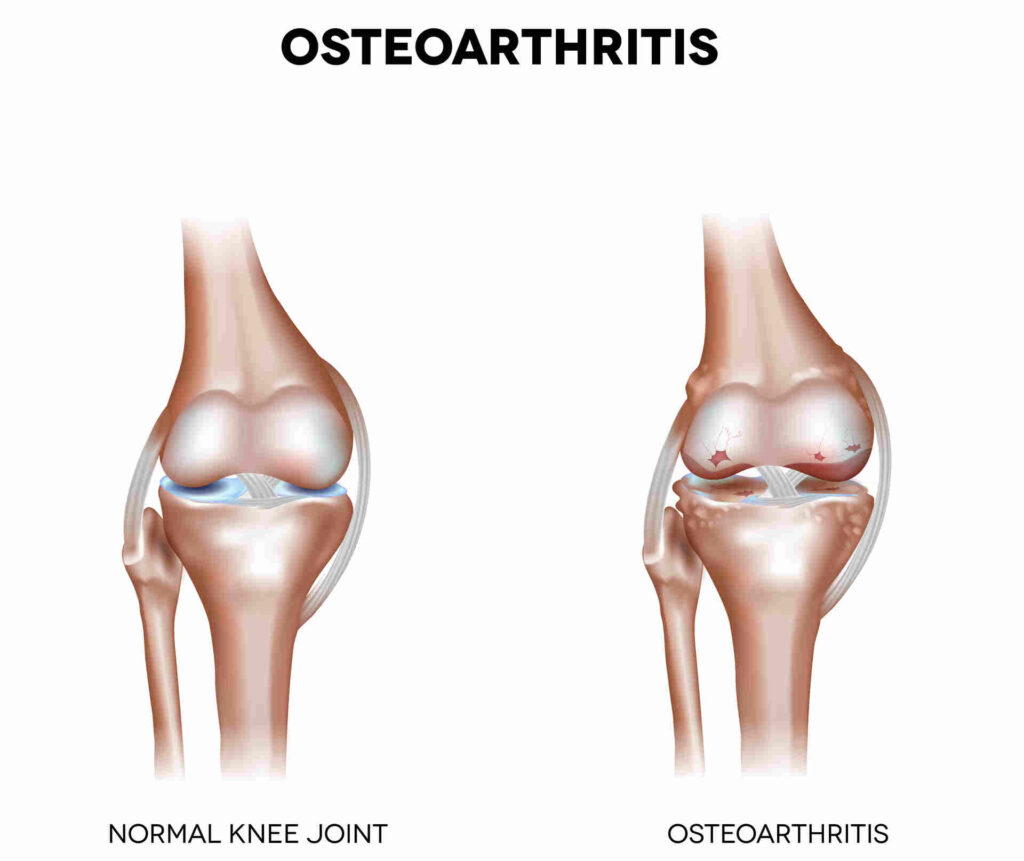
- Knee pain relief
- Low back pain
- Tennis and golfer’s elbow
- Neck pain
- Impaired range of motion
- Whiplash, sports injuries
- Headaches
- Jaw pain
Conclusion
If you are curious about dry needling or acupuncture, ask your Peak Practitioner today about how it might benefit you! If you have any questions or are looking to try out dry needling or acupuncture, you can book a discovery call HERE to find out what a good option for you might be.















 What the research says:
What the research says: 



 My name is Helen, and I am a
My name is Helen, and I am a 
 It is characterized by pain in the lower back, hips, and/or pubic area that can be exacerbated by certain activities such as walking, climbing stairs, or even just standing for long periods of time. PGP can have a significant impact on quality of life.
It is characterized by pain in the lower back, hips, and/or pubic area that can be exacerbated by certain activities such as walking, climbing stairs, or even just standing for long periods of time. PGP can have a significant impact on quality of life.  The Fitsplint
The Fitsplint 
 For anyone out there wondering if it is safe to exercise during pregnancy, let me be the first to tell you YES, and it’s encouraged!
For anyone out there wondering if it is safe to exercise during pregnancy, let me be the first to tell you YES, and it’s encouraged!  Squat with a Ball
Squat with a Ball  Birddog
Birddog Leg lifts
Leg lifts
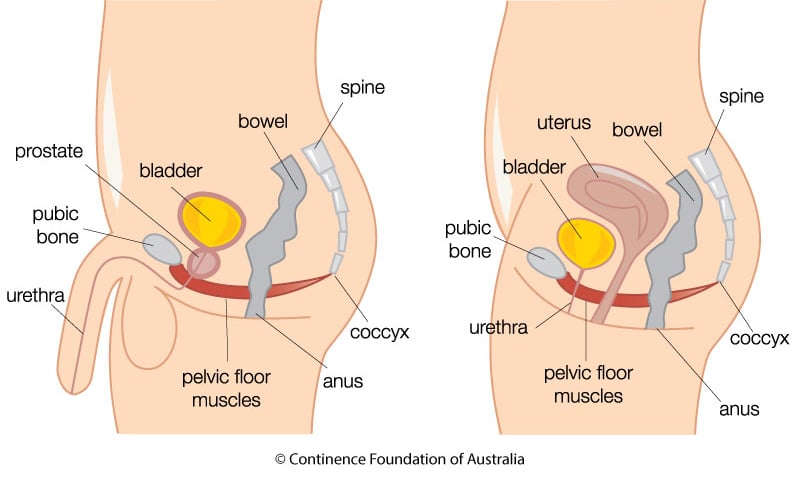
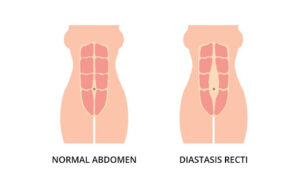 Rectus Diastasis:
Rectus Diastasis:  So…Who Should See a Pelvic Floor Physiotherapist?
So…Who Should See a Pelvic Floor Physiotherapist?